Images are a powerful component of health communication that are often employed to discourage risky behaviors. In particular, research indicates that gross visual representations of disease sources are effective in steering humans away from them (Curtis, 2004). For example, when cases of infectious disease rose in the 19th century, public health campaigns used disgusting images of rotting food and germ transmission as a tactic to promote disease-avoidance behaviors, such as hand washing and eating thoroughly cooked meat (Perry, 2016). At the turn of the 21st century, the World Health Organization (WHO) found that “globesity – an escalating global epidemic of overweight and obesity” affected 200 million adults and another 18 million under-five children worldwide (World Health Organization, 2013). Since then, public health campaigns in hundreds of nations have shifted much of their focus from communicable disease rates to the rapid emergence of obesity, but the usage of revolting images in health communication strategy remains unchanged.
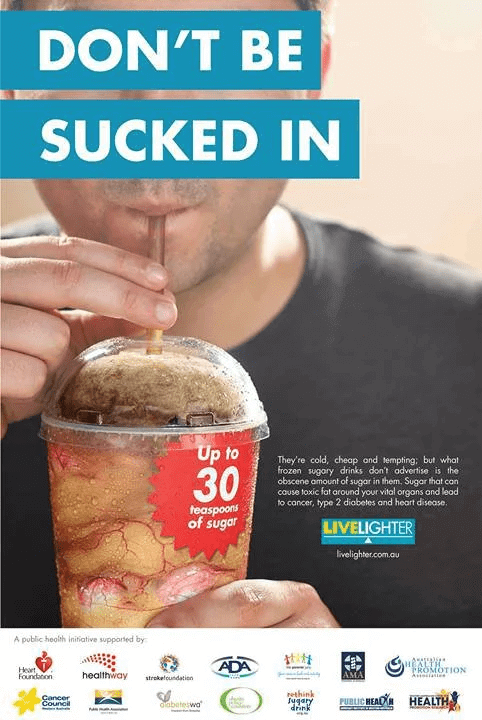
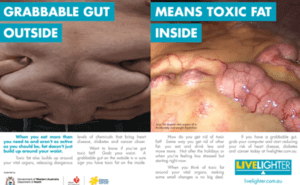 Just as previous advertising elicited pathogen disgust, many anti-obesity campaigns promote moral disgust through upsetting visuals to discourage unhealthy consumption behaviors. For example, in 2012 the Australian campaign LiveLighter released an advertisement series titled Toxic Fat, one of which depicts a man reaching for a slice of pizza late at night and grabbing the folds of his stomach in the process. This is accompanied by a shot of the inside of his gut, displaying visceral fat – slimy, yellow lumps of adipose accumulation around his internal organs. Another add features a man drinking a sugary cola—filled with slimy intestines. Not only is the fat itself and the likelihood of co-morbid disease disgusting, but through association, the man himself is implied to be disgusting as well. Overall, the commercial’s gross images sparked controversy as some argued for its benefit while others protested its fatphobic agenda. Facebook even blocked the advertisements by this campaign, indicating that they violated their policy against ads “that reference body images in a way that may make some viewers upset” (O’Leary, 2017).
Just as previous advertising elicited pathogen disgust, many anti-obesity campaigns promote moral disgust through upsetting visuals to discourage unhealthy consumption behaviors. For example, in 2012 the Australian campaign LiveLighter released an advertisement series titled Toxic Fat, one of which depicts a man reaching for a slice of pizza late at night and grabbing the folds of his stomach in the process. This is accompanied by a shot of the inside of his gut, displaying visceral fat – slimy, yellow lumps of adipose accumulation around his internal organs. Another add features a man drinking a sugary cola—filled with slimy intestines. Not only is the fat itself and the likelihood of co-morbid disease disgusting, but through association, the man himself is implied to be disgusting as well. Overall, the commercial’s gross images sparked controversy as some argued for its benefit while others protested its fatphobic agenda. Facebook even blocked the advertisements by this campaign, indicating that they violated their policy against ads “that reference body images in a way that may make some viewers upset” (O’Leary, 2017).
On one hand, some health communications professionals argue that using revolting images with moralizing implications is an effective strategy because the guilt appeal functions as a motivator. By perpetrating feelings of unease, shame, fear, and self-loathing, graphic visuals create incongruence between a consumer’s existing and ideal state, which should drive behavioral change (Hullett, 2004). Here, the method of inspiring disgust as a persuasion tactic is based on the assumption that an individual is driven by a need to appease their guilt (Hullett, 2004). Therefore, images evoking self-conscious emotions may be an efficient strategy in combating obesity. A 2015 study on different advertisement tactics in anti-obesity campaigns offers some support for this claim. Of all the advertisements included in the study, Toxic Fat was the only ad that fell into the “graphic execution” category and found to be the most effective in eliciting an emotional response for participants with a BMI of at least 25 (Dixon, 2015). Instead of tracking behavioral changes, which would require exposure to advertisements over time, this study examined the strength of short-term emotional and cognitive engagement. The investigators found that participants who viewed Toxic Fat were more willing to acknowledge their overweight status and the necessity of a lifestyle change. Thus, this study suggests a relationship between feelings of discomfort and ad effectiveness in impacting consumer perception (Dixon, 2015).
On the other hand, many researchers question the relationship between revolting imagery, disgust, and positive health outcomes. BMI is the parameter for weight categorization and the variable targeted by anti-obesity campaigns, but it is a crude indicator of health. BMI is a mathematical function of the “average person’s” height and mass (Gutin, 2017). Its validity is inflated as an average person does not exist – BMI ranges and their implications are not generalizable to a demographically diverse population (Gutin, 2017). So, if not an uptick in population health, what do fat-shaming public health campaigns actually accomplish? Many weight and health communication researchers contend that they stigmatize people who are overweight, ultimately doing more harm than good for everyone. Research shows that obesity stigma does not support healthy behavior, but drives negative emotions such as self-loathing, which can increase the frequency of erratic or abnormal consumption patterns (Tomiyama, 2015). Thus, linking health only to weight may cause larger people to feel so much shame that they are embarrassed to diet or exercise, while thinner people may feel it doesn’t matter whether they make healthy choices or create obsessions with avoiding weight-gain that result in eating disorders like anorexia (Freeman, 2011). Furthermore, by linking feelings of disgust with weight to individual morality, these campaigns reduce weight-related issues to apolitical solutions like diet, exercise, and sometimes clinical intervention, when the focus should really be on addressing the sociological roots of ill health, such as poverty and racism.
Obesity discourse has recently been shaped by what many see as a resurgent fatphobia during the COVID-19 pandemic. Obesity has been identified as a major risk factor for COVID-19 hospitalization (JHU Coronavirus Resource Center, 2020). While the dangers of anti-fat bias in healthcare long precede this pandemic, medical fatphobia is particularly dangerous now because overweight individuals receive poorer care and suffer worse outcomes than their normal and underweight counterparts (Tomiyama, 2018). In a society that already marginalizes fat bodies, graphic advertisements can reify fatphobic norms and perpetuate tangible harms. On the other hand, some scholars justify these advertising efforts by highlighting their marginal success in obesity prevention and population health promotion. Health communication and public health officials must continue to question the ethical implications surrounding the crux of anti-obesity campaigns and their use imagery evoking disgust.
Discussion Questions:
- What are the ethical values and conflicts involved in public health efforts promoting imagery evoking disgust?
- What are the consequences of stigmatizing fatness? Could you make an argument that such fat shaming is bad, even if it convinced people to shed weight?
- Would the benefits of slowing the obesity epidemic outweigh the social and emotional harms caused by this kind of advertising? If not, what emotional appeals might be more ethical?
- How far can health communication campaigns go in using emotions to motivate healthier behavior? What ethical principles should guide or limit such tactics?
Further Information:
Curtis, V., Aunger, R., & Rabie, T. (7 May 2004). Evidence that disgust evolved to protect from risk of disease. Proceedings of the Royal Society of London. Series B: Biological Sciences, 271(Suppl_4). doi:10.1098/rsbl.2003.0144
Dixon, H., Scully, M., Durkin, S., Brennan, E., Cotter, T., Maloney, S., & Wakefield, M. (20 August 2015). Finding the keys to successful adult-targeted advertisements on obesity prevention: An experimental audience testing study. BMC Public Health, 15(1). doi:10.1186/s12889-015-2159-6
Freeman, D. (3 May 2011). Are Georgia’s anti-obesity ads unfair to fat kids?. CBS News. Available at: https://www.cbsnews.com/news/are-georgias-anti-obesity-ads-unfair-to-fat-kids-pictures/
Gutin, I. (25 October 2017). In BMI we trust: Reframing the body mass index as a measure of health. Social Theory & Health, 16(3), 256-271. doi:10.1057/s41285-017-0055-0
Hullett, C. R. (August 2004). Using Functional Theory to Promote Sexually Transmitted Disease (STD) Testing. Communication Research, 31(4), 363-396. doi:10.1177/0093650204266103
O’Leary, C. (12 July 2017). Facebook rejects WA’s LiveLighter ‘grabbable gut’ advert. PerthNow. Available at: https://www.perthnow.com.au/news/wa/facebook-rejects-was-livelighter-grabbable-gut-advert-ng-3832d307d4e68ed26001eaed2d130ce0
Perry, S. (1 August 2016). To get us to wash our hands, public-health campaigns may need to elicit more disgust. MinnPost. Available at: https://www.minnpost.com/second-opinion/2016/08/get-us-wash-our-hands-public-health-campaigns-may-need-elicit-more-disgust/
Tomiyama, A. J., Carr, D., Granberg, E. M., Major, B., Robinson, E., Sutin, A. R., & Brewis, A. (15 August 2018). How and why weight stigma drives the obesity ‘epidemic’ and harms health. BMC Medicine, 16(1). doi:10.1186/s12916-018-1116-5
World Health Organization. (6 December 2013). Controlling the global obesity epidemic. World Health Organization. Available at: https://www.who.int/nutrition/topics/obesity/en/
Authors:
Neha Dronamraju, Kat Williams, & Scott R. Stroud, Ph.D.
Media Ethics Initiative
Center for Media Engagement
University of Texas at Austin
March 15, 2021
Images: livelighter.com.au
This case was supported by funding from the John S. and James L. Knight Foundation. These cases can be used in unmodified PDF form in classroom or educational settings. For use in publications such as textbooks, readers, and other works, please contact the Center for Media Engagement.
Ethics Case Study © 2021 by Center for Media Engagement is licensed under CC BY-NC-SA 4.0